Screening for social determinants of health is increasingly being recognized as an important element of whole-person care in clinical settings. There is a growing diversity of tools available that can be tailored to specific contexts and patient needs.
For example, a cluster RCT has recently examined the impact of integrating a poverty screening and service referral approach into routine well-child visits.
Education
The quality and availability of education is a key driver of health outcomes. For example, adults with low levels of education report poorer self-rated health, infants born to mothers without a high school degree die at higher rates, and individuals with higher levels of educational attainment live longer than those with less education.
Screening for social risk factors like education can help to identify and refer patients to interventions at the community level to address these determinants of health, such as family home visitation programs that reduce child maltreatment or tenant-based rental assistance programs. However, champions of the field rightly point out that addressing these factors requires action at the broader structural and political level, not just screening.
Frontline clinicians can be important advocates and catalysts of these broader efforts to create supportive environments for health at both the community and systemic levels, locally and nationally.
Employment
During the COVID-19 pandemic, the need for states to collect work and employment data became apparent. In fact, research has found that work is a significant social determinant of health and can be an indicator of an employee’s overall well-being.
A lack of stable employment can lead to food and housing instability, which in turn leads to poorer overall health. This vicious cycle is exacerbated by medical debt, as many Americans struggling with financial stress are also dealing with healthcare-related expenses.
One hospital system developed a protocol to screen for SDOH across its emergency departments using an eHR tool, standardized screening questions, a culturally sensitive Patient Navigator workforce, and trusted community partnerships. The result was a measurable impact on patients’ lives.
Housing
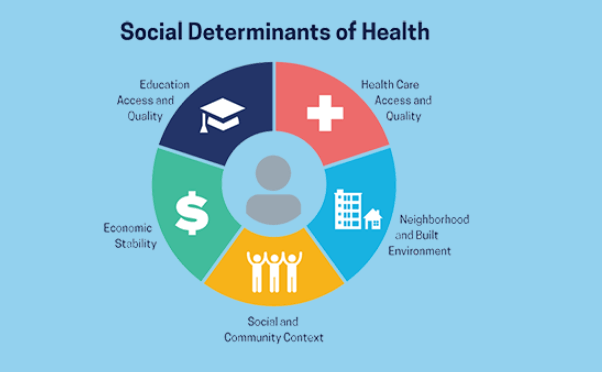
In addition to a patient’s medical history, their socio-economic status can have a significant impact on their health. These non-medical factors, known as social determinants of health, can be grouped into five categories: housing, economic stability, food and water security, access to education, and transportation.
This first systematic review catalogs housing questions asked of families in clinical and social service settings determines validated screening tools, and extracts information on recommendations for action following the screening. Heterogeneity in study design, age ranges, and the precise wording of housing questions across studies limits direct comparison.
However, with the increasing emphasis on value-based payment, healthcare organizations are in a unique position to identify and address unresolved social needs that can have a profound impact on health outcomes. Several screening tools are available, and the ICD-10 “Z” codes can help identify and document these needs.
Transportation
Over the last decade, there has been a growing body of literature on screening for social determinants in clinical care. There are multiple tools available to identify single dimensions of social risk such as intimate partner violence, poverty and financial security, access to child care, education, housing quality and affordability, and mental health (see Table 1).
While some studies have shown that screening for these factors is associated with improved outcomes, there is limited evidence on the impact of interventions that address them. Some advocates of social determinants argue that screening is not the right level of intervention and that broader intersectoral and whole of government approaches are needed to change the systemic and structural forces that influence the health and well-being of communities.
Read also How Woolworths Loblawsgray
Mental Health
The environment can have a huge impact on one’s mental health. It can influence the safety of one’s neighborhood, the schools they attend, the availability of green space, and other social goods. People are also more likely to suffer from mental health problems in an environment filled with stigma. People need to talk about their struggles and seek professional help from a counselor, psychiatrist or psychologist.
Screening tools typically focus on specific mental health conditions or symptoms, potentially overlooking other relevant factors in an individual’s mental well-being. Screening is an initial step but does not replace a comprehensive evaluation by qualified professionals. Moreover, many screening tools have limited validity and reliability. This is a critical challenge in developing effective mental health screening strategies.